Health care providers who deliver culturally responsive care are aware of and sensitive to these diverse values, beliefs, and behaviors. Receiving culturally responsive care is associated with better health outcomes and more positive experiences with the health care system.
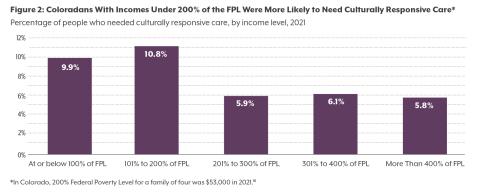
According to the 2021 Colorado Health Access Survey (CHAS), about one in 14 (6.9%) Coloradans reported needing health care that was responsive to a particular need or part of their identity, most often due to their disability, language, sexual orientation, or experience with violence or abuse.
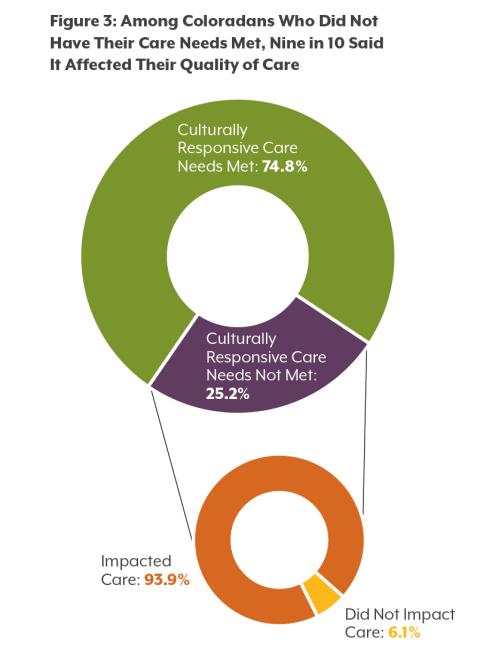
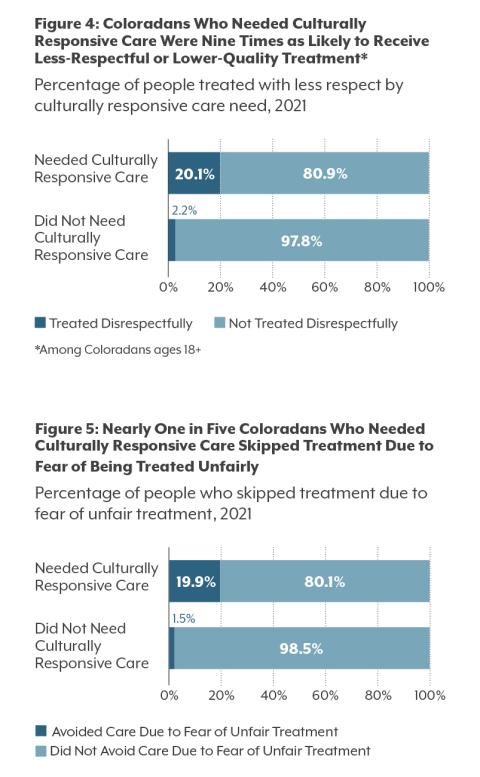
People who reported that their identity or personal history made a difference in the care they needed were more likely to report being treated with less respect by health care providers. They were also more likely to avoid getting health care when they needed it due to their fear of being treated unfairly.
Colorado providers and policymakers are working to strengthen fluency in culturally responsive care across the health care workforce, but they can do more to ensure that the health care system meets the unique needs of all Coloradans.
The Need for Culturally Responsive Care
According to the 2021 CHAS, an estimated 388,000 Coloradans needed culturally responsive care. The most common reasons people reported for needing this care were disability status, experience with abuse or violence, language, and/or sexual orientation (see Table 1). CHI’s work in stigma and health equity leads us to believe that this is very likely an undercount, indicating that many more Coloradans need some form of culturally responsive care than are reflected in the data. Additionally, those who need culturally responsive care due to characteristics like refugee status or experiences with homelessness are likely being undercounted. The CHAS is only administered to those with home mailing addresses and is only offered in English and Spanish, which means this data excludes people experiencing homelessness and people who speak neither English nor Spanish, two groups that are likely to need culturally responsive care.
Intersectionality in Health Care
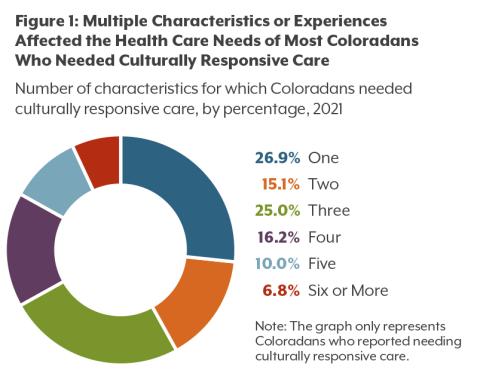
Nearly three out of four people who needed culturally responsive care reported that more than one characteristic affected the care they needed; more than half reported at least three. Some Coloradans identified six or more characteristics that made a difference in the care they needed (see Figure 1).
How the Colorado Health Access Survey Defines Culturally Responsive Care and Discrimination
To understand Coloradans’ need for culturally responsive care, CHI asked the following questions in a series. This brief defined those who answered “yes” to the first question as needing culturally responsive care. Our definition of culture is expansive and includes socioeconomic factors and personal histories that can guide health decisions.
- Does your language, race, religion, ethnic background, culture, gender identity, sexual orientation, disability, or other personal history, such as domestic violence or refugee status, make a difference in the kind of health care you need?
- Which of the following makes a difference in the kind of care you need: language other than English; race; religion; ethnic background or culture; gender identity; sexual orientation; a disability or physical, mental, or cognitive condition; experience with violence or abuse (such as domestic violence); experience with homelessness; asylum seeker or refugee status; other (specify)? Respondents could choose as many responses as they felt appropriate.
- In the last 12 months, have all of your health care providers met those needs?
- Thinking back to the health care providers who did not meet your needs, did your experience with them impact your ability to get the care you needed or the quality of care you received?
- The CHAS also asked respondents who were 18 and older about discrimination in the health system. While this concept is related to culturally responsive care, this question focused on experiences in the health care system, as opposed to health care needs. The question was:
- In the last 12 months when seeking health care, did you feel you were treated with less respect or received services that were not as good as what other people get?
These overlapping experiences and identities affect the type of care people needed. One common set of factors that combined to affect the health care Coloradans needed is language, culture, and race. Of people who said that the language they speak affected their health care needs, 43.5% also reported needing culturally responsive care due to their culture and 38.3% due to their race.
The most common reason people reported needing culturally responsive care on the 2021 CHAS was a disability. Of this group, 39.6% reported that their history with abuse or violence affected the care needed and an additional 22.1% reported sexual orientation also affected their health care needs. Some people who needed culturally responsive care due to a disability also reported that their gender identity (17.5%) or their experiences with homelessness (15.2%) affected their needed care.
To offer comprehensive culturally responsive care, providers need to incorporate intersectionality — the notion that different identities can overlap and interact to create unique experiences, such as privilege, disadvantage, or discrimination — when providing care to patients, understanding that many dynamics shape their patients’ experiences and needs.
In the United States, people with disabilities are disproportionately likely to be victims of abuse or to experience homelessness. The same is true for LGBTQ people, particularly youth and youth of color. Providers need to be aware that their patients’ experiences affect the care they need and their perceptions of or trust in the health care system. Similarly, in treating LGBTQ Coloradans with disabilities, doctors providing intersectional, culturally responsive health care must consider not only how sexual orientation and disability can independently impact patients’ health care needs but also how those overlapping identities can affect the care that patients need. For instance, research has found that LGBTQ patients with disabilities often face additional difficulties within the health care system because they have to “come out” multiple times to providers — by explaining both their disability and their sexual orientation — and navigate multiple identities when seeking care.